17 June 2024 | Monday | News
Picture Courtesy | Public Domain
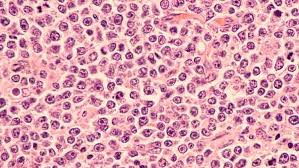
Positive results from the ECHO Phase III trial showed AstraZeneca’s CALQUENCE®(acalabrutinib) in combination with bendamustine and rituximab demonstrated a statistically significant and clinically meaningful improvement in progression-free survival (PFS) and showed a favorable trend in overall survival (OS) compared to standard-of-care chemoimmunotherapy (bendamustine plus rituximab) in previously untreated patients with mantle cell lymphoma (MCL).
These results were presented in a late-breaking oral presentation at the European Hematology Association (EHA) 2024 Hybrid Congress in Madrid, Spain (#LBA3439).
Results showed the CALQUENCE combination regimen reduced the risk of disease progression or death by 27% compared to standard-of-care chemoimmunotherapy (hazard ratio [HR] 0.73; 95% confidence interval [CI] 0.57-0.94; p=0.016). Median PFS was 66.4 months for patients treated with the CALQUENCE combination (n=299) versus 49.6 months with standard-of-care chemoimmunotherapy (n=299).
The secondary endpoint of OS showed a favorable trend for the CALQUENCE combination compared to standard-of-care chemoimmunotherapy, further supporting the clinical benefit of this combination (HR 0.86; 95% CI 0.65-1.13; p=0.2743). The OS data were not mature at the time of this analysis and the trial will continue to assess OS as a key secondary endpoint.
The ECHO trial enrolled during the pandemic period, and a pre-specified analysis censoring for COVID-19-related deaths was conducted to assess the impact. PFS was further improved in both arms, with the CALQUENCE combination reducing the risk of disease progression or death by 36% (HR 0.64; 95% CI 0.48-0.84; p=0.0017). Median PFS was not reached among patients treated with the CALQUENCE combination versus 61.6 months for standard-of-care chemoimmunotherapy (HR 0.64; 95% CI 0.48-0.84; p=0.0017). A favorable trend was seen for OS in this analysis for the CALQUENCE combination (HR 0.75; 95% CI 0.53-1.04; p=0.0797).
Michael Wang, MD, Puddin Clarke Endowed Professor, Director of Mantle Cell Lymphoma Program of Excellence, Co-Director of Clinical Trials at MD Anderson Cancer Center in Houston, US and principal investigator in the trial, said: “For people living with mantle cell lymphoma, a typically aggressive form of non-Hodgkin's lymphoma, the ECHO results offer promise of a new, effective treatment option for adults older than 65, who represent the majority of MCL patients. The improved progression-free survival seen in patients treated with the CALQUENCE combination compared to chemoimmunotherapy demonstrate its potential to change the standard of care as the only BTK inhibitor in this first-line setting.”
Susan Galbraith, Executive Vice President, Oncology R&D, AstraZeneca, said: “The ECHO trial data demonstrate important progress in improving outcomes for patients with mantle cell lymphoma. The 16.8 months of additional time patients can live without their disease progressing is highly clinically meaningful, together with a trend to improvement in overall survival. We therefore believe CALQUENCE plus chemoimmunotherapy will be an important new option for patients living with this disease.”
Summary of Results: ECHO
|
|
CALQUENCE plus bendamustine and rituximab (n=299) |
Placebo plus bendamustine and rituximab (n=299) |
|
Median PFS (months) |
66.4 |
49.6 |
|
PFS HR (95% CI) |
0.73 (0.57-0.94) |
|
|
PFS p-value |
0.0160 |
|
|
OS HR (95% CI) |
0.86 (0.65-1.13) |
|
|
OS p-value |
0.2743 |
|
|
Censoring for COVID-19 deaths |
||
|
Median PFS |
NR |
61.6 |
|
PFS HR (95% CI) |
0.64 (0.48-0.84) |
|
|
PFS p-value |
0.0017 |
|
|
OS HR (95% CI) |
0.75 (0.53-1.04) |
|
|
OS p-value |
0.0797 |
|
|
NR=Not reached |
||
The safety and tolerability of CALQUENCE was consistent with its known safety profile, and no new safety signals were identified. Grade 3 or higher adverse events (AEs) due to any cause occurred in 88.9% (n=264) of patients treated with the CALQUENCE combination and 88.2% (n=262) of patients treated with standard-of-care chemoimmunotherapy, including Grade 3 or higher atrial fibrillation in 3.7% (n=11) and 1.7% (n=5) of patients, Grade 3 or higher hypertension in 5.4% (n=16) and 8.4% (n=25), Grade 3 or higher major bleeding in 2.0% (n=6) and 3.4% (n=10), and Grade 3 or higher infections in 41.1% (n=122) and 34.0% (n=101), respectively. Serious AEs and Grade 5 events were balanced across arms (69% [n=205] versus 62% [n=184], and 12.1% [n=36] versus 10.1% [n=30], respectively). AEs leading to discontinuation were observed in 10.4% (n=31) and 6.4% (n=19) of patients for the CALQUENCE combination and placebo arms respectively. AEs related to COVID-19 were seen in the trial, including Grade 5 events which occurred in 9.4% (n=28) of patients treated with the CALQUENCE combination and 6.7% (n=20) of patients treated with standard-of-care chemoimmunotherapy.
Additional AstraZeneca data at EHA
In addition to these compelling data, AstraZeneca data at EHA 2024 shows how the Company is advancing a diverse and innovative pipeline spanning multiple modalities including next-generation T cell engagers, cell therapy and antibody drug conjugates, to enable the creation of novel combination regimens across a range of blood cancers.
Results from the ongoing Phase I, dose-escalation trial of AZD0486, a novel CD19xCD3 T cell engager, showed durable responses in patients with heavily pretreated relapsed/refractory follicular lymphoma with a median follow up of 11 months. Complete response rates of 84% were seen at doses of AZD0486 of 2.4 mg and above. Data also showed how cytokine release syndrome (CRS) events were effectively mitigated by the double step-up dosing schedule and no immune effector cell-associated neurotoxicity syndrome (ICANS) events were observed.
In an oral presentation, preliminary data was shared from an investigator-initiated trial of AstraZeneca’s first hematology cell therapy, GC012F (AZD0120), in patients with transplant-eligible high-risk, newly diagnosed multiple myeloma. Early results showed that GC012F had an overall response rate of 100%, a minimal residual disease-negative stringent complete response rate of 95%, and was well tolerated. Grade 1-2 CRS was experienced by 27% (6/22) of patients and no ICANS or neurotoxicity was observed. GC012F is a novel BCMAxCD19 dual-targeting autologous chimeric antigen receptor T therapy (CAR-T) created using the next-day FasTCAR manufacturing platform pioneered by Gracell Biotechnologies, a wholly owned subsidiary of AstraZeneca.
© 2026 Biopharma Boardroom. All Rights Reserved.