10 December 2024 | Tuesday | News
Picture Courtesy | Public Domain
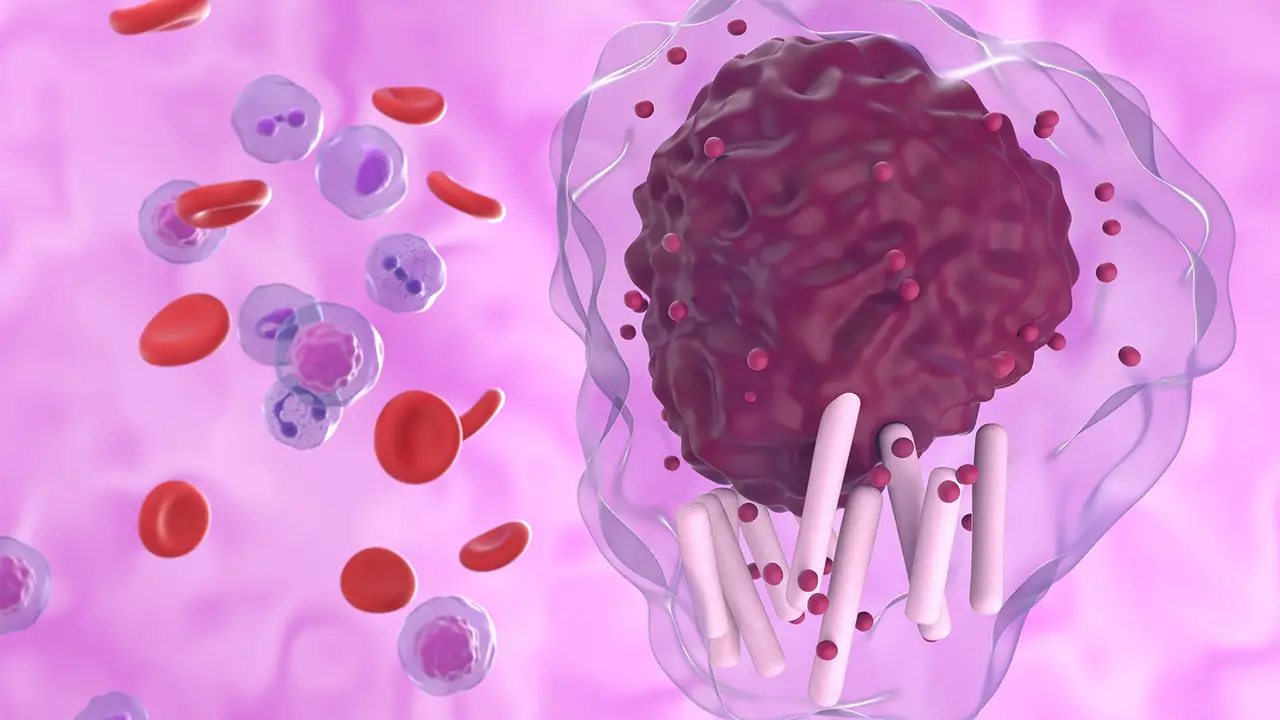
Eli Lilly and Company (NYSE: LLY) announced results from the Phase 3 BRUIN CLL-321 trial evaluating pirtobrutinib, a non-covalent (reversible) Bruton's tyrosine kinase (BTK) inhibitor in adult patients with chronic lymphocytic leukemia or small lymphocytic lymphoma (CLL/SLL) previously treated with a covalent BTK inhibitor. The study's primary endpoint of progression-free survival (PFS) was met at primary analysis1, demonstrating pirtobrutinib was superior to investigator's choice of idelalisib plus rituximab (IdelaR) or bendamustine plus rituximab (BR), based on independent review committee (IRC) assessment. Today's updated results corresponding to the final prespecified analysis, demonstrate consistent improvement in PFS for patients treated with pirtobrutinib, with a reduction in risk of relapse, disease or death by 46% compared to IdelaR or BR. These data will be presented in an oral presentation at the 66th American Society of Hematology (ASH) Annual Meeting and Exposition.
"These results demonstrate the ability of pirtobrutinib to deliver clinically meaningful outcomes in a post-covalent BTK inhibitor setting, which is especially remarkable given the poor prognosis for the patient population enrolled in BRUIN CLL-321," said Jeff Sharman, M.D., Disease Chair, Lymphoma Research Executive Committee, SCRI at Willamette Valley Cancer Institute and Research Center, and one of the principal investigators of the BRUIN CLL-321 trial. "These data also show that pirtobrutinib can significantly prolong the time to next treatment with a median of approximately two years. Coupled with the safety results, the BRUIN CLL-321 data are important as we consider treatment sequencing for this setting."
BRUIN CLL-321 enrolled 238 patients who were randomized to receive pirtobrutinib monotherapy (n=119) or investigator's choice of IdelaR or BR (n=119). Patients across both arms received a median of three prior lines of therapy, with all patients having received at least one prior covalent BTK inhibitor. Approximately half of the patients had also received a venetoclax-containing regimen. Reflective of the poor prognosis of patients enrolled in this study, a high proportion of patients presented with high-risk features indicative of aggressive disease, including TP53 mutation and/or 17p deletion, unmutated IGHV status and complex karyotype.
Efficacy results are based on IRC assessment of the intent-to-treat (ITT) population and utilize an Aug. 29, 2024 data cutoff date. Crossover to the pirtobrutinib arm was allowed after IRC-confirmed disease progression. At median follow-up of approximately 19 months, median PFS was 14.0 months for the pirtobrutinib arm compared to 8.7 months for the control arm (HR=0.54 [95% CI, 0.39-0.75]). PFS results were consistent across key subgroups associated with a poor prognosis, including patients who received prior venetoclax and those with TP53 mutations and/or 17p deletions, unmutated IGHV status and complex karyotype.
Pirtobrutinib also demonstrated clinically meaningful improvements in other secondary endpoints such as investigator-assessed PFS (median PFS: 15.3 vs. 9.2 months; HR=0.48 [95% CI, 0.34-0.67]), event-free survival (EFS) (median EFS: 14.1 vs. 7.6 months; HR=0.39 [95% CI, 0.28-0.53]), and time to next treatment (TTNT) or death (median TTNT: 23.9 vs. 10.9 months; HR=0.37 [95% CI, 0.25-0.52]). Specifically, among patients in the control arm who were eligible for crossover, 76% (n=50/66) crossed over to receive pirtobrutinib. Multiple analyses that adjust for the effect of crossover demonstrate trends in favor of pirtobrutinib (Inverse Probability Censored Weighting methodology: HR= 0.89 [95% CI, 0.52-1.53]; two-stage Accelerated Failure Time methodology: HR=0.77 [95% CI, 0.45-1.26]).
The overall safety profile for patients treated with pirtobrutinib in BRUIN CLL-321 was consistent with safety data from the Phase 1/2 BRUIN study, including adverse events of special interest. In the Phase 3 study, pirtobrutinib treatment was associated with fewer grade 3 or higher treatment-emergent adverse events (TEAEs) and fewer treatment discontinuations due to adverse events compared to IdelaR or BR. When adjusting for exposure, the incidence rate of TEAEs was overall lower in patients receiving pirtobrutinib compared to IdelaR or BR.
"BRUIN CLL-321 is the only randomized CLL or SLL study ever conducted exclusively in the BTK-inhibitor pre-treated population, where there is significant need for new treatment options, and these data illustrate pirtobrutinib's ability to meaningfully delay disease progression and time to next treatment in this setting," said David Hyman, M.D., chief medical officer, Lilly. "This is the first in our suite of randomized Phase 3 trials for pirtobrutinib to readout and we look forward to continuing to build the body of evidence supporting the role of pirtobrutinib in advancing care for people with B-cell malignancies."
Lilly is committed to the ongoing investigation of pirtobrutinib in people living with hematologic malignancies. The BRUIN clinical trial program consists of six clinical studies, four of which are Phase 3 studies evaluating pirtobrutinib in CLL/SLL. For more information on the BRUIN Phase 3 clinical trial program, please visit clinicaltrials.gov.
Pirtobrutinib is approved as Jaypirca® under the U.S. Food and Drug Administration's (FDA) Accelerated Approval pathway for the treatment of adult patients with CLL/SLL who have received at least two prior lines of therapy, including a BTK inhibitor and a B-cell lymphoma 2 (BCL-2) inhibitor and adult patients with relapsed or refractory mantle cell lymphoma (MCL) after at least two lines of systemic therapy, including a BTK inhibitor. These indications are approved under accelerated approval based on response rate. Continued approval for these indications may be contingent upon verification and description of clinical benefit in a confirmatory trial.
© 2026 Biopharma Boardroom. All Rights Reserved.